Road of recovery in gastrointestinal surgery: From ERAS to FRAS
Published 14 May, 2024
In the 1990’s Dr. Henrik Kehlet introduced the concept of enhanced recovery after surgery (ERAS), pioneering multimodal surgical care. Initially applied to patients undergoing colonic surgery, ERAS has also been dedicated to developing multimodal perioperative care to improve patients' recovery after major surgery through research, education, audit and implementation of evidence-based practice, aiming to close the “knowing-doing” gap. Representing a paradigm shift in perioperative care. ERAS challenges traditional practices, replacing them with evidence-based best practices in perioperative care.
Currently, the debate has shifted away from whether colorectal surgery following ERAS principles or traditional care is superior, towards enhancing the approach and streamlining its implementation. One such improvement involves transitioning patients from a surgical procedure requiring a 3-4 day hospital stay to a 1-2 day, or even same-day outpatient visit.
To this end, a team of researchers from China proposed a new concept called fastest recovery after surgery (FRAS) and implemented it in clinical practice to expedite recovery in patients undergoing elective major gastrointestinal surgery, building upon existing ERAS protocols.
“FRAS is a series of strengthened multimodal perioperative care pathways to optimize physiologic function, minimize surgical stress response, improve response to stress, and facilitate fastest postoperative recovery with improving comfort and satisfaction,” explains Xiaohuang Tu, co-corresponding author of the study.
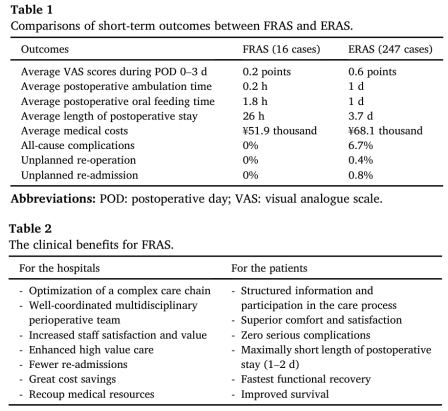
The researchers conducted pilot studies comparing short-term outcomes between FRAS and ERAS, and found that FRAS demonstrated “zero” complications; significantly reduced hospital stay duration; substantial cost savings and notably superior perioperative comfort and satisfaction (Table 1 and Table 2).
The team reported their study in the KeAi journal Gastroenterology & Endoscopy.
“Considering the evidence underpinning the recommendations is continuously evolving, clinical guidelines need to be challenged and updated on a regular basis. More clinical evidence from high quality of randomized controlled trials or real-world medical data with large sample size are needed,” notes Tu.
Contact author details:
Xiaohuang Tu, Department of Gastrointestinal Surgery, Shanghai Fourth People's Hospital, School of Medicine, Tongji University, Shanghai, 200434, China, tuxiaohuang@126.com.
Funder:
The authors were partially supported by National Natural Science Foundation of China (82130121, 82293640, and 82293643 to L.X.), China Postdoctoral Science Foundation (2023M732654 to H.W.), Medical Scientific Research Foundation from Hongkou District Health Commission (Hongwei2302-18 to N.Z., Hongwei2302-21 to J.C.), and Scientific Research Foundation from Shanghai Fourth People's Hospital (sykyqd04401 and sykyqd05101 to X.T., sykyqd04801 and SY-XKZT-2022-1002 to G.C.).
Conflict of interest:
Drs. Huanghui Wu, Qizhi Liu, Nan Zhang, Junyi Chen, Guozhong Chen, Lize Xiong, Xiaohuang Tu have no conflicts of interest or financial ties to disclose.
See the article:
Huanghui Wu, Qizhi Liu, Nan Zhang, Junyi Chen, Guozhong Chen, Lize Xiong, Xiaohuang Tu, Road of recovery in gastrointestinal surgery: From ERAS to FRAS, Gastroenterology & Endoscopy, Volume 2, Issue 2, 2024, Pages 84-89, https://doi.org/10.1016/j.gande.2024.03.007.